The Evolution of Stents: How Far Have We Come?
 When your arteries are narrowed or blocked, this can sometimes be a wellness warning of a heart attack. These days, a stent can fix that problem, and the little device has come a long way to be able to do so, but there was a time when cardio doctors thought they could live without them.
When your arteries are narrowed or blocked, this can sometimes be a wellness warning of a heart attack. These days, a stent can fix that problem, and the little device has come a long way to be able to do so, but there was a time when cardio doctors thought they could live without them.
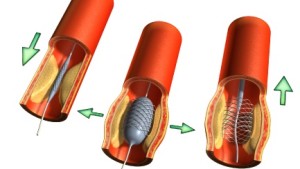
An angioplasty is a procedure to widen narrowed or obstructed arteries and it used to be done without any stents. The first angioplasty on a coronary artery was performed in 1977, in Zurich, Switzerland, by Dr Andreas Gruentzig, a German-born physician. Back then, the surgeon would stretch the artery with an inflated balloon, and the balloon would be removed along with the fine guidewire. However, as vessel walls are elastic in nature, and therefore tend to spring back or recoil after the procedure, this, coupled with the formation of scar tissue, meant that restenosis could occur, in which your treated vessel becomes blocked again.
Clearly, something had to be done and so bare metallic stents were introduced in 1986. According to Dr Benjamin Chua, the director of endovascular surgery and a consultant at the department of general surgery at the Singapore General Hospital, stents act as struts, radiating force outwards to keep arteries open. However, though these devices solved one problem, they created other issues too.
Because bare stents exert an outward force against the arterial walls, extensive scar tissues grow inside the device, causing your blood flow to be obstructed. This can affect your wellbeing with symptoms such as chest pain, and so the next evolution of stents was born: drug-eluting stents. These stents are coated with medication, which is released over time to stop your body from responding to injury, and causing restenosis.
Though each new stent reduced restenosis by up to 20% each time, there was still a problem with thrombosis, or clotting, which can occur from within 24 hours to a year later and is more common with drug-coated stents. People who have bare stents have to take two kinds of blood-thinning or anti-clotting medication for at least a month while those with drug-coated stents have to take both for at least a year.
So, we come to the last evolution of stent: biodegradable drug-eluting stents, which remove the root causes of vessels narrowing after a procedure, but do not remain permanently to trigger extensive scar tissue growth. Also known as the Absorb stent, Dr Goh Yew Seong, a consultant at the department of cardiology at Changi General Hospital, explained, ‘Although the Absorb stent’s premise of leaving nothing behind is an attractive option for most patients, we must still be stringent in lesion selection in order to ensure the best outcome.’


Comments are closed.